PQRS 2017 (January 3, 2017)
CMS has officially discontinued the PQRS and rolled all the measures therapists were reporting into the new Quality Payment Program (QPP). Therapists are not eligible participants in this program for 2017; however, therapists can continue to voluntarily report the same PQRS measures they were reporting in 2017. There will be no financial reward or punishment for not reporting, but the advantage is that you will generate a yearend report that provides feedback on your success rate for reporting. This could help confirm you are meeting the reporting threshold for successfully reporting once therapists are included (anticipated in 2019). If you reported via claims, you can continue to put the PQRS on your claims. If you reported via registry, you will have to check with the registry to see if they are still planning to continue reporting.
PQRS 2016 (February 19, 2016)
CMS has not made any changes to the measures or reporting requirements for 2016.
Please refer to the information and Quality Measures Charts for 2015 (located below) for 2016 reporting. Eligible therapists who do not successfully report all eligible measures on 50 percent of their Medicare beneficiaries will see a 2-percent payment reduction in 2018.
CMS has added a new tool for looking up the requirements for reporting each of the PQRS measures.
PQRS codes (January 13, 2015)
The following table is a quick reference for PQRS codes and measures eligible for submission by individual practitioners submitting PQRS data via claims based reporting. ASHT recommends that providers review the documentation requirements for each measure published by CMS.
2015 PQRS Individual, Claims Reported Measures- PT and OT
2015 PQRS Individual Claims Reported Measures- OT only
Documenting PQRS Codes on the 1500 form (January 13, 2015)
The following recommendations apply to Hand Therapists who report PQRS measures via Claims reporting on the 1500 form.
- CMS recommends that the PQRS codes are reported on the lines following the eligible reporting CPT code. (Typically 97001, 97003, 97002, 97004)
- For PT's the PQRS codes should be submitted on the line under the evaluation code, then the PQRS codes should be on the lines under the FLR codes.
- PQRS codes should not be submitted with the GP, GO or KX modifiers. For some codes, modifiers 1P or 8P may be applied.
- The diagnosis pointer column should be filled in, typically with 1.
- CMS recommends that a charge of .01 be submitted in column F.
- Column G should have a "1" in it.
- Any other CPT codes for treatment should follow or be submitted on an additional form.
(Example only, treatment dates, diagnosis codes and NPI would be included.)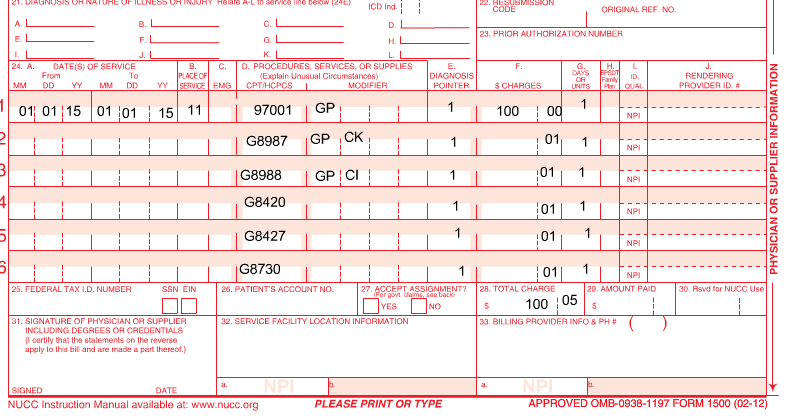
Legislative Alert - PQRS 2015 for Hand Therapists (December 5, 2014)
CMS has issued PQRS reporting rules updates for 2015.
Background: PQRS is an outcome measure-reporting program using payment adjustments to encourage information reporting by eligible professionals on services covered by the Medicare Physician Fee Schedule furnished to Medicare beneficiaries under Medicare Part B (including Railroad Medicare and Medicare Secondary Payer). The goal is to improve the quality of data reporting in order to reduce claim fraud and ensure accurate reimbursement by CMS.
The ACA mandates the development of the NQS or National Quality Strategy. The mission is to promote improved individual health care and reduce healthcare costs. CMS established these NQS domains based on those goals:
- Patient and Family Engagement
- Patient Safety
- Care Coordination
- Population and Public Health
- Efficient Use of Healthcare Resources
- Clinical Processes/Effectiveness.
PQRS measures fall under 1 or more of these categories. Reporting should include codes in three domains to demonstrate a wider range of data.
PQRS Updates for 2015
Eligible providers face a penalty of -2% in 2017 if they do not report on covered professional services furnished to Medicare part B fee for service beneficiaries successfully.
PQRS participation in 2016 is also tied to a new program: Value-Based Modifier Program (VM) that starts for therapy practices in 2018. Data collected in 2016 will be subject to additional financial penalties or incentives in 2018 payments. This program is separate from, but tied to PQRS reporting. Failure to participate in 2016 PQRS reporting will affect the VM program and could result in 4% reduction of Medicare payments in 2018 based on 2016 reporting. This reduction will be in addition to the 2% reduction for not reporting or unsuccessful reporting of PQRS in 2016. More information on the VM program will be posted in the near future.
Reporting
All therapists billing under Medicare Part B Physician Fee Schedule for outpatient therapy services in private practices are eligible to report PQRS.
Therapists who work in facility or institutional outpatient clinics who bill under Medicare Part A are not eligible. Rehab agencies, Outpatient Hospitals, SNF's, Part B federally qualified health centers, rural health clinics or ambulatory surgery centers are paid under different methodologies and are not eligible to report PQRS. They use the UB-92 (UB-04) or 8371 for billing and these forms do not have a space for reporting individual NPIs.
Methods for reporting
Reporting can be either claims or registry. There is a fee to contract with the registry. Registries track compliance and reporting rate and remind the provider to report in order to be compliant. Data can be submitted retrospectively through the registry. Claims reporting does not require a fee, but the provider must be diligent with reporting and track their own compliance rate. Data must be reported on the claim and cannot be submitted retrospectively.
Registry-based, individual provider: Providers contract with a CMS-approved registry. The provider selects the PQRS measures to track. The registry submits this data to CMS for the provider. No registration with CMS required.
Registry based, Group practice (GPRO): Practices with two or more providers must sign up with CMS to report under one tax ID. Must register with CMS to report under this option by June 2015.
2015 Registry Reporting Requirements
Group option 1
The reporting individual or group must report nine measures covering three National Quality Strategy (NQS) domains for 50% of Medicare eligible patients.
These measures must include reporting on one cross cutting measure (more on this below) and 2 outcomes measures. If two are not available, one outcome measure and one of the following types of measures may be reported: resource use, patient experience of care, efficiency/appropriate use.
If less than nine measures are applicable to the reporting professional, 1-8 measures covering the three domains must be reported. Individuals reporting less than nine measures will be subject to an additional review: the MAV process. (More below on this process.)
There are eight eligible measures across four NQS domains for PTs and 10 for OTs submitting individual reporting through a registry.
Group option 2
The group must report six measures across two NQS domains, including one cross cutting measure on 50% of Medicare Part B patients and have a CMS certified survey vendor complete a Consumer Assessment of Healthcare Providers Systems or CAHPS on behalf of the practice.
Group option 3
Reporting through CMS' web interface. This option is available for practices of 25 + providers: The group must report on all measures included in the interface for their first 248 Medicare Part B patients. If they have less than 248, they must report on al least one measure for 100% of their Medicare Part B patients. Practices reporting through the Web interface are not subject to the MAV process. All the data must be entered manually.
Groups with more than 100 providers must also add a CAHPS survey component no matter which reporting method they choose.
Claims based, individual reporting: The provider determines which measures to track and submits the code for each measure on their claim form for each appropriate visit based on the measures specifications. PQRS data cannot be submitted retroactively-it must go in on the original claim.
2015 Claims Reporting
Despite the fact that the majority of participants submit via claims reporting,
CMS has announced it has made plans to eliminate claims reporting in the future. (Registries charge a fee for their services, so once claims reporting is eliminated, providers will have to pay for the privilege of participation.)
For 2015, individual providers can continue to report via claims. For PTs, only six measures across three NQS domains are available to report via claims reporting, four of these are cross cutting measures. In this case, the reporting provider will be subject to an additional process, the MAV process (detailed below).
(Those practices participating in FOTO reporting have additional registry reporting measures available to them. FOTO measures are not listed in the chart below.)
For OTs, nine measures across three NQS domains are available to report via claims reporting, five are cross cutting and should be reported.
Measure Applicability Validation Process: When there are not nine measures that are applicable to the provider, a new review process will be triggered. This allows CMS to determine whether an eligible professional should have reported quality data codes for additional measures or NQS. Due to the lack of eligible measures, PTs will all be subject to this process. OTs who do not report nine measures will also be subject to this process. To date, PTs do not need to take any additional action as the process will be triggered automatically and the claims will be reviewed.
Cross Cutting Measures: Cross cutting measures are clinical quality measures (CQM) that are broadly applicable. They are intended to provide CMS with quality data on more varied aspects of an eligible professional's practice. CMS plans to require more cross cutting measure reporting in the future.
2015 Reporting Measures
|
Meas. #. |
Measure Description |
OT |
PT | Cross-Cutting | Registry | Claims |
NQS (National Quality Strategy) |
| 128 | BMI | x | x | x | x | x | Population Health |
| 126 | Diabetes Foot/Ankle Evaluation | x | x |
Effective Clinical Care |
|||
| 127 | Diabetes -Footwear Evaluation | x | x |
Effective Clinical Care |
|||
| 130 | Documentation of Current Medication ns in the Medical Record | x | x | x | x | x | Patient Safety |
| 131 | Pain Assessment and Follow-Up | x | x | x | x | x | Population Health |
| 134 | Preventative Care and Screening: Screening for Clinical Depression and Follow-Up Plan | x | x | x | x | Community/Population Health | |
| 154 | Falls Risk Assessment | x | x | x | x | Patient Safety | |
| 155 | Falls POC | x | x | x | x | Care Coordination | |
| 173 | Alcohol Consumption Assessment | x | x | Health | |||
| 181 |
Elderly Maltreatment Screen and Follow-Up |
x | x | x | Patient Safety | ||
| 182 | Functional Outcome Assessment | x | x | x | x | x | Care Coordination |
| 226 | Tobacco Use Screen and Cessation Intervention | x | x | x | Community/Population Health |
Eliminated measures from 2014
245: Use of wound surface culture technique in patient with chronic skin ulcers
148-1515:Back pain measures group
The measure specifications for the 2015 PQRS codes are available and can be found here.
Scroll to the lower 1/3 of the page and download the zip file: "2015 PQRS Individual Claims Registry Measure Specification Supporting Documents." The first document in the file lists the 2015 measure specifications. Refer to the PQRS information posted on our Legislative Resources Page under Updates from ASHT to locate the applicable measure number.
For more information on 2015 PQRS, please visit CMS.gov.