The Functional Reporting requirements of reporting the functional limitation non-payable HCPCS G-codes and severity modifiers on claims for therapy services and the associated documentation requirements in medical records have been discontinued, effective for dates of service on and after January 1, 2019
FUNCTIONAL DATA COLLECTION FOR MEDICARE OUTPATIENT THERAPY
What is it?
Who will be impacted?
What is a G code?
How often does the FLR codes need to be reported?
When does it take effect?
What are the basics a therapist must understand about functional reporting?
What if a client is only seen for one visit?
What if the client is seen by more than one discipline in one day i.e. OT and PT?
What should be documented in the medical record?
What if the client is seen for an orthosis only and billed using an L-code?
Who can document this information?
How does this affect submitting claims to Medicare and use of the KX modifier?
Can the functional reporting be completed using an electronic fee ticket and electronic health record?
Client Example
Helpful Resources
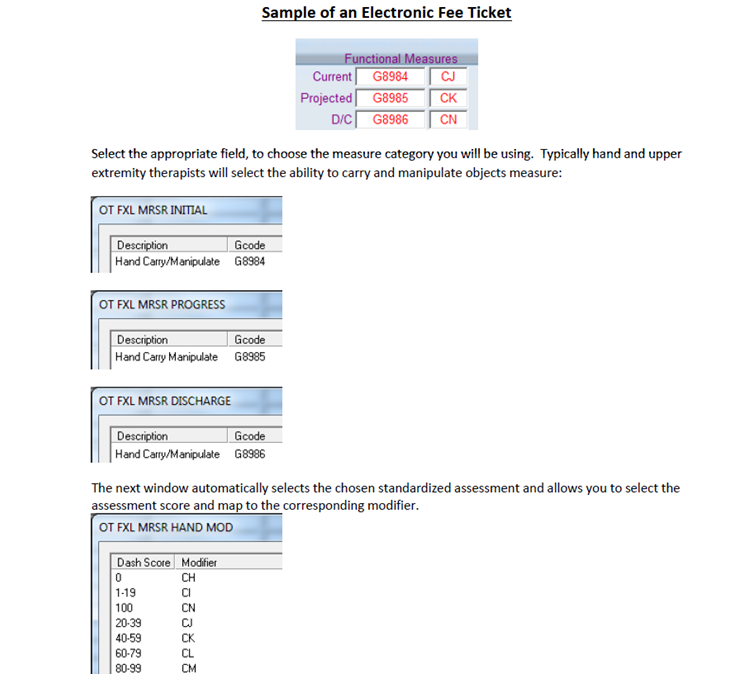
Sample of an Electronic Fee Ticket
What is it?
As part of the Middle Class Tax Relief and Jobs Creation Act, a claims-based system to collect data for outpatient therapy services is being developed. The stated objective is that this data will be used to develop an improved Medicare payment system.
Who will be impacted?
All providers billing outpatient therapy services under the Medicare Part B programs including:
- Outpatient therapy clinics including hospital out-patient centers
- Private practice: physician and non-physician owned
- CORFs
- SNFs
- Rehabilitation agencies
- Home health
- Services provides “incident to” physician services
- Critical access hospitals
What is a G code?
A G code is part of a coding system used to communicate information about a client’s functional status to Medicare on the claim form. The G codes are not used to bill for services. Instead, they are used to communicate information about the client’s functional impairment. G codes will also be used in the Physician Quality Reporting System or PQRS.
How often does the FLR codes need to be reported?
It is required that the data be reported:
- At the time of initial evaluation
- Every 10 treatment visit or when a re-evaluation is billed
- At discharge
- If finished reporting on one functional limitation and beginning to report on another
When does it take effect?
After July 1, 2013, Medicare will no longer accept claims that do not have the required functional data and G codes.
The data collection system went into effect January 1, 2013 but this period of time through June 30, 2013 is considered a testing period for the new system.
What are the basics a therapist must understand about functional reporting?
There are four main components of the FLR code functional reporting system. A therapist must be able to answer the following four main questions in reporting functional data for an individual client. These questions include the following which are discussed in detail below:
- On which set of functional FLR codes will I report?
- Do I need to report on current status, projected goal status or discharge Status?
- Which discipline specific modifier will I be using?
- How will I report severity/complexity modifiers?
1. On which set of functional FLR codes will I report?
There are 6 FLR code sets which are more typically used by OT and PT. An example of a set of FLR codes is Mobility: Walking and Moving Around. Another set of FLR codes is Self-Care. Click here for a full list of the sets reported by PT or OT and for guidelines on choosing the appropriate FLR code.
There are 42 functional FLR codes, 14 sets of 3 codes each. Generally, 6 of the FLR code sets would typically be used by PT and OT to address functional limitations:
Of the 6 sets typically reported for PT or OT:
4 sets are for categorical functional limitations:
- Mobility: Walking & Moving Around
- Changing & Maintaining Body Position
- Carrying, Moving and Handling Objects
- Self Care
2 sets are for “Other” functional limitations:
- Other PT/OT Primary
- Other PT/OT Subsequent
(A separate set of eight FLR codes is available that would not typically be used in hand therapy. They address communication and swallowing issues more frequently addressed by SLPs or therapists working in those treatment areas.)
The therapist must choose the FLR code considered to have the greatest relevance to the client’s clinical care or report on the primary reason the client is being seen in therapy. The client’s priorities for therapy and which areas are expected to result in the greatest or fastest improvements should also be considered when selecting the FLR code set upon which to report.
The “other” codes can be used in several different circumstances.
- When treatment is designed to address a limitation that is not a functional limitation, such as wound care or the treatment of lymphedema.
- When the clients functional limitation does not fit into the categories provided
- When the outcome score used to report the functional limitation does not meet the categories provided.
Only one functional limitation is reported at a time. If further therapy is needed when reporting on one functional limitation has ended, the therapist will need to begin reporting on a different set of FLR codes.
2. Do I need to report on current status, projected goal status or discharge status?
There are different requirements for reporting from the FLR code set during the reporting periods. Each of the functional sets of FLR code set contains a code for each of the following:
- Current status
- Projected Goal Status
- Discharge Status
This is an example of a set of FLR codes:
Carrying, Moving & Handling Objects
G8984 Carrying, moving & handling objects functional limitation, current status, at therapy episode outset and at reporting intervals
G8985 Carrying, moving & handling objects functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting
G8986 Carrying, moving & handling objects functional limitation, discharge status, at discharge from therapy or to end reporting
At the time of the initial evaluation, 2 codes must be reported:
- current status
- projected goal status
At the time of re-evaluation or at reporting intervals (usually every 10 treatment sessions), 2 codes must be reported:
- current status
- projected goal status
At the time of discharge, 2 codes must be reported:
- projected goal status
- discharge status
To end reporting of a one functional limitation, the discharge status must be reported on the original status while the current status and projected goal status must be reported on the new functional limitation.
For a full list of FLR codes see http://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnmattersarticles/downloads/MM8005.pdf
3. Which discipline specific modifier will I be using?
OT, PT and SLP each have their own modifier.
The FLR code also needs to include a modifier based upon which discipline is providing services:
- GP – under a PT plan of care (POC)
- GO – under an OT POC
- GN – under an SLP POC
4. How will I report severity/complexity modifiers?
Each non-payable functional FLR code must include one of the severity/complexity modifiers listed below. The severity modifier reflects the client’s percentage of functional impairment and must be reported with each FLR code. Along with clinical judgment, a therapist should use a functional assessment tool or other performance measurement instrument to determine the impairment limitation.
Modifier Impairment Limitation Restriction
CH 0 percent impaired, limited or restricted
CI At least 1 percent but less than 20 percent impaired, limited or restricted
CJ At least 20 percent but less than 40 percent impaired, limited or restricted
CK At least 40 percent but less than 60 percent impaired, limited or restricted
CL At least 60 percent but less than 80 percent impaired, limited or restricted
CM At least 80 percent but less than 100 percent impaired, limited or restricted
CN 100% impaired, limited or restricted
A free tool to convert a client’s score on an outcome assessment to the appropriate severity modifier is available at http://www.mediserve.com/resource/analysis/cbor-conversion/
If reporting on a client whose therapy does not treat a functional limitation the FLR code used should be the “other” set and the severity code should be entered as zero or CH.
The order of modifiers does not matter and the severity modifier and the discipline modifier must be reported with each functional FLR code.
What if a client is only seen for one visit?
The therapist reports on all 3 G code sets for that visit.
What if the client is seen by more than one discipline in one day i.e. OT and PT?
Four G code sets would be reported instead of the usual two.
What should be documented in the medical record?
Documentation in the medical record should reflect the functional outcome tool used, the score, and must support the modifier selection.
What if the client is seen for an orthosis only and billed using an L-code?
Functional reporting is not required when billing L-codes only.
Who can document this information?
A qualified occupational or physical therapist directly providing services or providing services incident to a physician can document. A physician or NPP furnishing services can also document.
How does this affect submitting claims to Medicare and use of the KX modifier?
When submitting a claim form, do not append the 59 or KX modifier to the G codes. Include it on a separate and distinct line. No specific order of modifiers is required. Claims should have a $0.00 on the claim form unless an amount is required. In that case, an amount a $0.01 is advised.
Can the functional reporting be completed using an electronic fee ticket and electronic health record?
Yes, an electronic health record and fee ticket can be valuable to streamline and simplify the process along with helping to ensure compliance with the functional reporting requirements. An example is included at the end of this document.
Client Example
The G code set most relevant to the client’s care is determined to be Carrying, Moving & Handling Objects and the functional outcome tool used is the DASH. An OT evaluation is completed and the client score on the DASH is a 65. The OT’s clinical judgment expects that the client’s DASH score will improve to between 20 and 40 within the next reporting period (10 visits including the initial evaluation).
Two sets of codes would be reported at the initial evaluation:
- G8984 GO CM
- G8985 GO CK
G8984 Carrying, Moving & Handling Objects functional limitation; current status
G0 Therapy specific modifier for OT
CM Severity/complexity modifier at least 60 percent but less than 80 percent impaired, limited or restricted
G8985 Carrying, moving & handling objects functional limitation, projected goal status
GO Therapy specific modifier for OT
CK At least 20 percent but less than 40 percent impaired, limited or restricted
At the time of re-evaluation or after 10 visits, the DASH assessment is repeated and the clients score improves to 37. The therapist determines that it is reasonable to expect further progress and anticipates the client’s DASH score will improve to between 1 and 20 within the next reporting period.
Two sets of G codes would be reported at re-evaluation:
- G8984 GO CK
- G8985 GO CI
G8984 Carrying, Moving & Handling Objects functional limitation; current status
GO Therapy specific modifier for OT
CK Severity/complexity modifier at least 20 percent but less than 40 percent impaired, limited or restricted
G8985 Carrying, moving & handling objects functional limitation, projected goal status
GO Therapy specific modifier for OT
CI At least 1 percent but less than 20 percent impaired, limited or restricted
At time of discharge the client’s DASH score improves further to 15. The therapist determines the client has reached maximum improvement:
Two sets of G codes would be reported at discharge:
- G8985 GO CI
- G8986 GO CI
G8985 Carrying, moving & handling objects functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting
GO Therapy specific modifier for OT
CI At least 1 percent but less than 20 percent impaired, limited or restricted
G8986 Carrying, moving & handling objects functional limitation, discharge status, at discharge from therapy or to end reporting
GO Therapy specific modifier for OT
CI At least 1 percent but less than 20 percent impaired, limited or restricted
Helpful Resources:
http://www.apta.org/payment/medicare/codingbilling/functionallimitation/
http://www.aota.org/News/AdvocacyNews/Func-Data-Collection-CY-2013.aspx
http://www.mediserve.com/resource/analysis/cbor-conversion/
http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R2622CP.pdf
http://www.cms.gov/Outreach-and-Education/Outreach/NPC/Downloads/FunctionalReportingNPC.pdf